Cancer Survivor Month: Danielle Gose’s Story
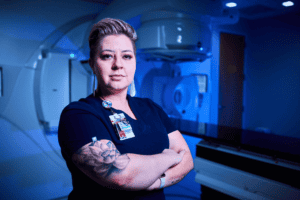
Danielle Gose, OCSRI Radiation Therapist
June is National Cancer Survivor Month, and OCSRI is honoring the journeys of those who have navigated the adversities of cancer diagnosis and treatment. Each survivor’s journey is a testament to their resilience, strength and support of their communities and caregivers. OCSRI hopes that through their words, those currently battling cancer would be able to reflect, find inspiration and know they are not alone in their fight. Please join us as we uplift these survivors and their unique, profound stories, which remind us that life after cancer is not only possible but can also be filled with profound meaning, joy and purpose.
Introduction:
My name is Danielle—I am a radiation therapist at Oklahoma Cancer Specialists & Research Institute (OCSRI) and a breast cancer survivor. I’ve worked for OCSRI for 5 years and have been a radiation therapist for 7 years. I’ve always loved working in this field and felt that this is what I was called to do. Empathy is something I have always had and I felt as though I connected well with my patients. However, it wasn’t until I became a cancer patient that I truly understood what they go through.
Diagnosis:
I felt a lump in mid-2021, but assumed it was just another cyst, as I’d already had many cysts due to fibrocystic breast disease. After monitoring it for just over 6 months, I noticed that the lump seemed to be bigger, and I also noticed sharp, throbbing pains that would occur sporadically. I saw one of my primary care doctors, shared with her my timeline and symptoms and she did a physical exam. She told me that it wasn’t a concern unless it had “been a while,” in which I asked for her to define what “a while” means. “About 3-4 months,” she replied. Now knowing that she was not listening to me, I repeated the fact that it had been at least 6 months. I insisted on imaging, and she was reluctant to put in those orders, despite being a 34-year-old presenting with an oblong lump in my breast.
A couple weeks later, when I was getting my diagnostic ultrasound, the tech went quiet and excused herself from the room. After an excruciatingly long 3 minutes, she returned with a radiologist in tow. The radiologist examined the area of concern that caused the tech to become quiet, and that’s when I felt it: the strangely heavy cloud in the room, undoubtedly filled with sadness and fear for me. The radiologist sat down on the bed next to me and placed his hand caringly on mine as he told me that he would like to take a closer look and order a biopsy. Two weeks later, after what felt like an eternity, my biopsy day arrived. The morning after my biopsy, a nurse from my doctor’s office called me and told me, ever-so-casually, that I did indeed have cancer.
On January 13, 2022, at the age of 34, I was diagnosed with invasive ductal carcinoma. I soon found out that I have the BRCA2 gene mutation, putting me at a higher risk for breast cancer, ovarian cancer, pancreatic cancer and skin cancer. This is likely to be the reason for my diagnosis. My main tumor measured about 1.4cm and was surrounded by several small tumors, called “satellite nodules”, measuring up to 8mm each, scattered along a 10cm-long area around my main tumor.
Treatment:
My healthcare team came up with a plan and things started rolling—not to say things had not already been nonstop since my diagnosis. Being 34 and not having kids yet, fertility preservation was one of the first things on my agenda. That began immediately, thanks to Dr. Ahlering and the incredible staff at MCRM Fertility Clinic. By February 16th, I was in surgery to have my chemo port placed and on March 10th, I started chemo.
The evening after my first chemo was completely unexpected. When you do chemo, you’re told that you will have nausea, but until you experience the nausea associated with chemo, you don’t have an actual understanding of what nausea truly feels like. Thanks to medicines that combat nausea, I only experienced one truly horrific bout of nausea in which I couldn’t even move to sit up for approximately 6 hours. It took a couple days of trial and error, but my incredible healthcare team finally got me set up on a regimen of nausea medicines to make it manageable.

I completed 4 rounds of Adriamycin/Cytoxan and 12 rounds of Taxol from March 10th to August 12th. On September 14th, I was back in the OR undergoing a bilateral mastectomy with reconstruction. Two weeks after surgery, I began hormone therapy in the form of a daily medication called Tamoxifen. This is used to block my body’s estrogen receptors due to my breast cancer being hormone receptor positive. In January of 2023, I underwent my last breast surgery to complete my reconstruction process. A few short months later, I had a complication with Tamoxifen and was forced to stop taking that medication and move to a monthly injection called Zoladex (Goserelin) paired with a different hormone blocker called Anastrozole (Arimidex), taken daily.

Survivorship:
Today, after almost 2 years cancer-free, I continue with my hormone therapy and will for another 8 years. As a BRCA2 carrier, I continue with 6-month screenings for ovarian cancer until I undergo a complete hysterectomy. I also have regular bone scans, CTs, blood tests, monthly Zoladex injections, monthly appointments with my medical oncologist, and checkups with my other specialists to screen for the other cancers that BRCA2 leaves me at high risk for.
How My Journey Has Influenced My Perspective as a Radiation Therapist:
My cancer journey greatly impacted my perspective and ability to care for my patients as a radiation therapist. I have been able to truly understand what my patients go through, although radiation therapy was not a part of my cancer treatment. The empathy I have for my patients goes deeper than it did before, and I am able to support my patients in a different way than I had. I now understand the fears of the unknown, the waiting, the pain, the emotions, the constant scans and doctor’s appointments. I understand what it means to lose your hair and control over your own body. I’m very open about my survivorship and always happy to share with a patient who asks or seems like it might help them to know. My perspective has completely changed because of what I experienced through my journey, and I believe that is a blessing from God.
Forms of Support:
I was lucky enough to have a huge support system; I not only had my family and friends, but I also had my incredible coworkers and bosses. I traveled as a radiation therapist for 2 years and met some wonderful friends in the process. I ended up receiving care packages, flowers, phone calls and text messages from people in Arkansas, South Carolina, Wisconsin, Colorado and Alaska. The love that surrounded me in my time of need was something that kept me going.
My faith was even more instrumental to me in my journey. My cancer journey gave me the gift of truly knowing God. He was my source of strength, faith, and joy. I remember people commenting on how I seemed to be feeling better or have more energy, but I was actually exhausted, out of breath, and felt sick. It was God who gave me the energy to smile and be grateful for the air in my lungs and the heartbeat in my chest.
My coworkers and bosses were so amazing through it all. They surrounded me with such love and support, checked on me, gave me grace on my tough days, and worked with my chaotic schedule full of doctor’s appointments, scans, treatments and surgeries. I could not have done any of it without the support that they gave me.
Recommendations for Other Fighters:
Being a cancer fighter, and even survivor, comes with a lot of exhaustive days, side effects, emotions, fear, and need for support. The days are not always great, but they are not always bad either. It’s important to have a care team that you trust and can confide in. If you don’t trust your care team, then you need to find one you can.

It’s also important to be your own advocate or have someone you trust to be your advocate and stand up for your needs, beliefs, and, ultimately, your care. This became evident to me at the beginning of my journey when I had to push to get imaging done on a lump that had me concerned. I knew then that I would have to be ready to stand up for myself at any moment in my journey. I did just that when I switched breast surgeons, got a second opinion, asked all the questions I possibly could, and confided in my doctors with every symptom and side effect that I experienced.
You must be able to tell your team anything and everything that could possibly be related to your cancer or treatments. You never know when it’s something that needs to be known to ensure that you don’t have permanent health problems due to chemo, such as neuropathy, for example; or maybe it’s a symptom that tells your team that there is something that requires more imaging. It is your duty to yourself to inform your care team of anything new or unusual—they are not mind readers.
Importance of Early Detection & Regular Screenings:
I feel as though the importance of early detection speaks for itself, but as someone who didn’t initially believe that I had cancer, I understand the apprehension that a person might have when they notice something new or unusual on their body. It can be scary to face unknowns, making it seem as if it is just better to pretend it isn’t even a problem rather than potentially have a doctor give you news that you don’t want to hear.
It is important to me to make sure that people understand just how instrumental it is to be familiar with your own body and have regular screenings. If you are in tune with your body, then you might catch something potentially serious before it even becomes a problem. What do I mean by “being in tune with your body”? I mean being conscious of how your body normally feels. This gives you the ability to be aware of anything abnormal. This could be a new bump, lump, pain, rash, bleeding, et cetera. Whatever you don’t catch yourself can hopefully be caught early with regular screenings. This might be a physical exam, imaging, or other tests.
You never know when a scan might catch something you never even knew was there. My BRCA2 diagnosis led to my dad and sister finding out they also have the gene mutation. This discovery led to my dad’s sister being tested and finding out she had it, which led to my cousin finding out she also had it. Everyone immediately established genetic counselors and scheduled screenings and even preventative surgeries. My cousin had an abdominal CT scan that led to the discovery of a large mass on one of her kidneys. She went in for surgery almost immediately and is fine today, thankfully. She had no symptoms or reason to believe she had this large mass. It was purely a result of the cancer screening that it was even found.